Delirium – often described as “an acute brain dysfunction” observed to occur in over 25% of hospitalized patients. Delirium symptoms can vary from disorganized thinking, hallucinations, to drowsiness and have been classified in the literature as hypoactive, hyperactive, or mixed state.
Recognizing delirium is critical as it has shown to increase a patient’s likelihood of experiencing post-traumatic stress disorder, memory issues and cognitive impairments. Delirium can also lead to longer hospital stays, higher likelihood of hospital readmissions and can lead to an increased risk of death.
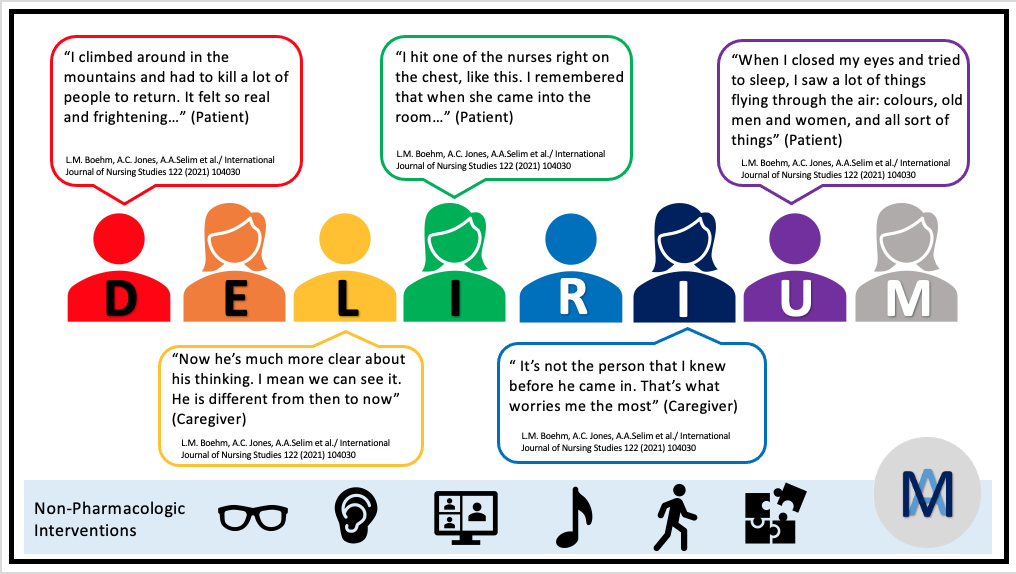
What is it like to experience delirium?
I was fortunate to have had an opportunity to meet and live with my great grandmother in my early childhood years. There used to be some occasions wherein she would wake up and describe that there is flooding in the house and that I should be standing on the bed instead of the floor. These thoughts would fluctuate, as often seen in patients experiencing delirium in the hospital. After some minutes, and reassurance and reorientation by my grandfather, she would “come back” from an episode of what I now think to have been “delirium”. As a young child, I remember being a little scared and confused on why my great grandmother was just not herself but quite “different”.
A recent study by Boehm et al. (2021) looked to synthesize previously published qualitative findings of patients and family experiences of delirium.
Few of the patients and caregivers quotes from this study:
Once delirium occurs. What should be done?
Over the years, clinicians and research scientists are pointing towards non-pharmacologic treatments over prescribing anti-psychotic medications.
Non-pharmacologic treatments that could potentially help include: providing patients with their glasses and hearing aids immediately post-surgery as to help with reorientation. Having family by the patient’s bedside, early mobilization, nutrition, and cognitively stimulating activities can are some options that have been identified in the literature as potential non-pharmacological delirium interventions.
World Delirium Awareness Day
Since the past few years, the second Wednesday of a full week of March has been allocated to recognizing delirium and bringing about its awareness in the World.
Clinicians across the world spend the day educating hospital staff about delirium and celebrate their team’s effort in recognizing, diagnosing and providing care for patients experiencing delirium.
Social media platforms like Twitter are used by clinicians and research scientists from around the world to promote World Delirium Awareness Day or WDAD, for short. Delirium organizations such as iDelirium, American Delirium Society, European Delirium Society and others join in by providing resources on delirium prevention, awareness and recognition.
Join in and celebrate the day of bringing awareness of delirium – a medical emergency, that impacts many individuals across the world. #WDAD2022.